 Wash your hands regularly and wear a face mask.
Learn more
Wash your hands regularly and wear a face mask.
Learn more
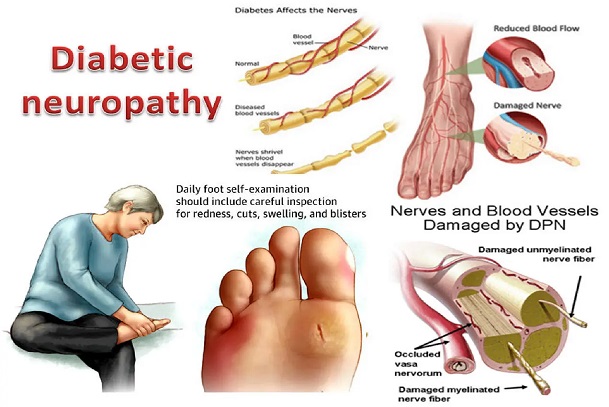
Diabetic neuropathy is a type of nerve damage that arise as a result of diabetes mellitus i.e., diabetes causing damage to the nerves. These damages can affect any type of nerves in the body including the organs, feet, legs, and muscles. It can cause pain and numbness in the legs, feet, hands, digestive system, urinary tract, blood vessels, heart, and disturbances.
Diabetic neuropathy is a serious diabetes complication that may affect as many as 50% of people with diabetes. But one can often prevent diabetic neuropathy or slow its progress with consistent blood sugar management and a healthy lifestyle.
There are several types of diabetic neuropathy and includes:
What Causes Diabetic Neuropathy?
Over time, uncontrolled high blood sugar levels from damage can damage the nerves throughout the body, interfering with the ability to send signals, leading to diabetic neuropathy/. High blood sugar also weakens the walls of the small blood vessels (capillaries) that supply the nerves with oxygen and nutrients. The higher the blood sugar levels, the more likely the damage to the nerves. Also, the older one gets and the longer one is diabetic, the more likely one is to experience nerve damage. People who have diabetes and drink too much alcohol are also more likely to have nerve damage. This can also cause peripheral neuropathy.
What are the Symptoms of Diabetic Neuropathy?
Symptoms of diabetic neuropathy depend on the nerves that have been damaged. There may be the inability to feel pain, especially in the feet which can lead to serious infections if sores and other problems are not treated.
The most common symptoms of diabetic neuropathy are numbness, tingling, a burning feeling, aching, weakness, and cramps, beginning in the feet or hands. These symptoms may later spread to the legs and arms. The loss of sensation on the foot ulcer leads to neuropathic ulcer due to the painless damage to tissues of the sole of the feet.
Other symptoms include autonomic neuropathy which causes:
What Are the Symptoms of Peripheral Neuropathy?
Peripheral neuropathy tends to develop slowly over months or years. In general, symptoms may include:
How Is Diabetic Neuropathy Diagnosed and Treated?
The doctor usually diagnoses diabetic neuropathy and peripheral neuropathy by performing a physical examination (by checking how a patient can feel light, touch, and temperature, testing the strength and reflexes) and carefully reviewing symptoms and medical history.
Along with the physical exams, the doctor can perform or order specific tests to help diagnose diabetic neuropathy and guide treatment, such as:
It is important to note that not all doctors can test for all types of nerve damage, so it is important to inform one’s doctor about any pain or weakness felt. Also, include heavy sweating or dizziness and any changes in digestion, urination, and sexual function.
Treatment
The goal of the treatment of diabetic neuropathy and peripheral neuropathy is to slow the progression of the disease, manage complications and restore functions while nerve pain is relieved.
This involves blood sugar level management. Consistently keeping the blood sugar within the target range is the key to preventing or delaying nerve damage (i.e., keeping the damage from getting worse, and the pain might get better). Good blood sugar management may even improve some of the current symptoms.
Other forms of treatment depend on each diabetic patient’s symptoms:
A diabetic patient may have a sore or other foot problem without noticing it, so it is important to check the feet every day. An untreated problem on the foot can lead to serious infection or foot ulcer which may lead to amputation. So, the patient needs to be clear with his/her doctor about what is helping him/her feel better and what is not. A patient and his/her doctor can work together to find the best treatment that helps the most.
Can Diabetic Neuropathy Be Prevented?
Diabetic Neuropathy and its complications can be prevented or delayed by managing one’s blood sugar levels within the target range and taking good care of the feet. This is best achieved by checking the blood sugar and adjusting treatment. It is also important to get to and stay at a healthy weight by exercising and eating healthy foods.
Can Peripheral Neuropathy Be Prevented?
Adopting healthy habits can reduce the effects of peripheral neuropathy. Eating a healthy diet, getting regular exercise, avoiding alcohol, and quitting smoking. Also, take care of the hands, feet, and legs by avoiding any form of injury. If HbA1C is kept at 6.0 or below, peripheral neuropathy can be prevented.
Diabetic Autonomic Neuropathy
Autonomic neuropathy occurs when there is damage caused by diabetes to the autonomic nerves that control automatic body functions. It can affect blood pressure, temperature control, digestion, bladder function, and sexual function. People with autonomic neuropathy may have one organ affected or it could affect several organs.
Examples of Autonomic Neuropathy
Gastroparesis: If blood sugar levels remain high over a long period, damage to the vagus nerve can occur. The vagus nerve is the nerve that controls the movement of food through the digestive tract. Gastroparesis happens when the vagus nerve is damaged or stops working. When this happens, the stomach takes longer than it usually does to empty its contents. This is called delayed gastric emptying. Symptoms of gastroparesis include nausea and vomiting, heartburn, feeling of fullness, bloating, loss of appetite, weight loss, and stomach spasms. Gastroparesis can make it more difficult to manage blood glucose levels since food absorption is less predictable. The best way to prevent gastroparesis is to manage blood sugar levels over time. Also, one can try to avoid eating high-fiber, high-fat foods, as they take longer to digest. Eating small meals throughout the day instead of fewer large meals can also help prevent gastroparesis.
Sexual Dysfunction: Autonomic neuropathy can also cause erectile dysfunction (ED) in men when it affects the nerves that control erection with sexual arousal. Having high sugar levels for some time can damage your blood vessels and nerves, including the ones that supply the penis. This can restrict the amount of blood flowing to the sexual organs, so one can lose some sensation. However, sexual desire does not usually decrease. One can get treatment for this with pills like Viagra and Cialis but seek a doctor’s advice before taking them, as they can cause heart problems. For women, sexual dysfunction is characterized by decreased moisture in the vagina and reduced sensation of the clitoris.
Heart and Circulatory System Problems: Diabetic autonomic neuropathy may damage the nerves in the heart and circulatory system, causing a sudden drop in blood pressure when one sits or stand up suddenly (orthostatic hypotension); rapid heart rate when one is not exercising (resting tachycardia); heart attack that causes no chest pain (silent heart attack).
Sweating and Temperature Regulation Problems: Autonomic neuropathy may affect the nerves that control sweating (reduced sweating), making it difficult to recognize when the blood sugar is dropping. Changes in the body's ability to regulate temperature may make one more prone to body chilling (hypothermia) or heat-related illness, such as heatstroke or heat exhaustion.
Digestive System Problems: Damage to the nerves of the stomach and intestines may cause constipation, because of abnormally slow passage of waste through the intestines; diarrhea, because of the abnormally fast passage of waste through the intestines. Diarrhea is more common at night; and belly pain.
What are the Symptoms of Autonomic Neuropathy?
Autonomic neuropathy may affect digestion, the body's ability to regulate temperature, urination, sexual function, and heart and blood vessel function, including blood pressure. In general, symptoms may include:
How Is Autonomic Neuropathy Diagnosed and Treated?
To diagnose autonomic neuropathy, a diabetic patient will need a physical exam and special tests as well. For example, an ultrasound test uses sound waves to check on the bladder. Stomach problems can be found using X-rays and other tests. Telling the doctor about one’s symptoms plays a big part in making a diagnosis and creating a better treatment plan.
Treatment
Treatment focuses on managing the symptoms of autonomic neuropathy. For example, taking medicines and eating small, frequent meals that are low in fiber and fat may help digestive problems like gastroparesis. Or you may take medicines for urinary or blood pressure problems. Medicines, lubricants, and creams may help with sexual problems.
Can Autonomic Neuropathy Be Prevented?
Autonomic neuropathy can be prevented by adopting a habit lifestyle, managing one’s blood sugar level within the right range (HbA1C < 6.0), having a healthy diet, getting regular exercise, and quitting alcohol and smoking.