 Wash your hands regularly and wear a face mask.
Learn more
Wash your hands regularly and wear a face mask.
Learn more
What Are the Long-Term Complications of Diabetes?
People with diabetes mellitus may experience serious, long-term complications that develop gradually. The longer the duration of diabetes, which is poorly controlled, the higher the risk of these complications which begins within months of the onset of diabetes, although most tend to develop after a few years and gradually worsen.
Possible long-term complications of diabetes mellitus include damage to the eyes, foot ulcer, and nerve damage (neuropathy).
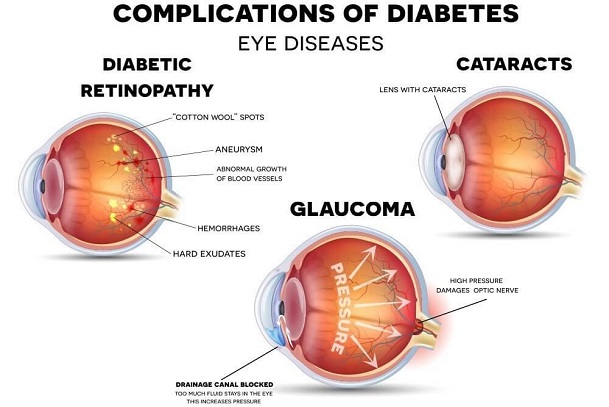
EYE DAMAGE (DIABETIC EYE DISEASES)
Diabetic eye disease is a group of eye problems that can affect people with diabetes. These conditions include diabetic retinopathy, diabetic macular edema (which usually develops along with diabetic retinopathy), cataracts, and glaucoma.
Damage to the eyes can lead to poor vision or even blindness. But early diagnosis and treatment can go a long way toward protecting one’s eyesight.
Diabetic Retinopathy
Diabetic retinopathy is caused when high blood sugar damages the blood vessels in the retina (a light-sensitive layer of cells in the back of the eyes). Damaged blood vessels can swell and leak, causing blurry vision or stopping blood flow. Sometimes, new blood vessels can grow abnormally and these can cause further vision problems, affecting both eyes.
Who is at Risk of Developing Diabetic Retinopathy?
Anyone with any kind of diabetes can get diabetic retinopathy - including people with type 1, type 2, and gestational diabetes (a type of diabetes that can develop during pregnancy). The risk increases the longer one has diabetes. Over time, more than half of people with diabetes will develop diabetic retinopathy, but the risk of developing diabetic retinopathy can be reduced by controlling one’s diabetes. Women with diabetes who become pregnant - or women who develop gestational diabetes - are at high risk for getting diabetic retinopathy.
What are the Symptoms of Diabetic Retinopathy?
A diabetic person can have diabetic retinopathy and not know it. This is because it often has no symptoms in its early stages. As diabetic retinopathy gets worse, one will notice symptoms such as:
How Is Diabetic Retinopathy Diagnosed and Treated?
Diagnosis
For diabetic patients, it is very important to get regular eye exams. If one does develop diabetic retinopathy, early treatment can stop the damage and prevent blindness.
Treatment
In the early stages of diabetic retinopathy, eye doctors will probably just keep track of how the eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months. In later stages, it is important to start treatment right away, especially if there are vision changes. Treatments such as:
How Can Diabetic Retinopathy Be Prevented?
Regular eye exams, good control of blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss. If one has diabetes, the risk of getting diabetic retinopathy can be reduced by doing the following:
Diabetic Macular Oedema
The part of the retina that helps a person see is referred to as the macula. Diabetes can lead to swelling in the macula, which is called diabetic macular edema. Over time, this disease can destroy the sharp vision in this part of the eye, leading to partial vision loss or blindness. Macular edema usually develops in people who already have other signs of diabetic retinopathy.
Cataracts
A cataract is the clouding of the normally clear lens in the eye. Though everyone’s lenses tend to get cloudy as they get older, people with diabetes are more likely to have cataracts, and at a younger age. Most cataracts develop slowly and don't disturb your eyesight early on. But with time, cataracts will eventually interfere with your vision.
It is usually caused by high blood sugar deposits building up in the lenses and making them cloudy most especially in diabetic persons. Other risk factors include high blood pressure, obesity, too much sun exposure over time, previous eye injury or inflammation and surgery, and smoking.
Who is at Risk of Developing Cataracts?
Anyone is at risk of developing cataracts as one gets older. But at higher risk, if one is diabetic; smokes; drinks too much alcohol; is having a family history of cataracts; had an eye injury, has eye surgery; or spends a lot of time in the sun.
Any Symptoms of Cataracts?
One might not have any symptoms at first when cataracts are mild. At first, the cloudiness in one’s vision caused by a cataract may affect only a small part of the eye's lens and one may be unaware of any vision loss. As the cataract grows larger, it clouds more of your lens and distorts the light passing through the lens.
This may lead to more-noticeable symptoms. One can also notice that:
How Are Cataracts Diagnosed and Treated?
To determine whether a patient has cataracts or not, a doctor may need to review the patient’s medical history and symptoms and perform an eye examination. There may be a need to conduct several tests, including:
Treatment
Surgery is the only way to get rid of a cataract, but you may not need surgery immediately until the cataracts are mature. After surgery (when the lens is removed), special eyeglasses are used. Modern surgery can put corrective lenses after removing the opaque lens in the eyes.
How Can Cataracts Be Prevented?
Certain conditions can be helpful in the prevention of cataracts, they include:
Glaucoma
Glaucoma is a group of eye diseases that causes blindness and vision loss by damaging a nerve in the back of the eye called the optic nerve. This damage caused is often related to high pressure in the eye, but glaucoma can happen even with normal eye pressure.
Glaucoma can happen to any person within any age group, but common among adults. It is one of the leading causes of blindness among people over the age of 60. This eye disease in most cases usually has no early symptoms but its effect is so gradual that one may not notice any change in vision until the condition is in its later stages.
Glaucoma in Children
A child may be born with glaucoma or develop it in the first few years of life. Blocked drainage, injury, or an underlying medical condition may cause optic nerve damage.
Who is at Risk of Developing Glaucoma?
Anyone can get glaucoma, but some people are at higher risk if they:
What are the Symptoms of Glaucoma?
At first, glaucoma doesn’t usually have any symptoms. This is most people with glaucoma do not know they have an eye disease. Over time, the person may slowly lose his/her vision, starting with patchy blind spots in one side vision (peripheral vision) that is closest to the nose. Then at later stages, difficulty seeing things in the central vision begins to occur. To diagnose it early, routine eye examinations like intraocular pressure should occur yearly after 40 years.
Other symptoms include severe headache, severe eye pain, blurred vision, nausea or vomiting, eye redness, and halos or colored rings around lights.
How Is Glaucoma Diagnosed and Treated?
A comprehensive eye examination is needed to diagnose the presence of glaucoma using tonometry to measure raised intraocular pressure found during the eye examination. Also, several other tests may be performed including:
Treatment
Early treatment and regular checkups can help slow or prevent vision loss, especially if the disease is diagnosed in its early stages. Such early treatment includes eye drops, oral medications, and surgery. Surgery is required in the late stages to reverse intraocular pressure.
How can Glaucoma be Prevented?
Glaucoma diagnosis and early management can help to prevent vision loss or slow its progress. The steps used include: