 Wash your hands regularly and wear a face mask.
Learn more
Wash your hands regularly and wear a face mask.
Learn more
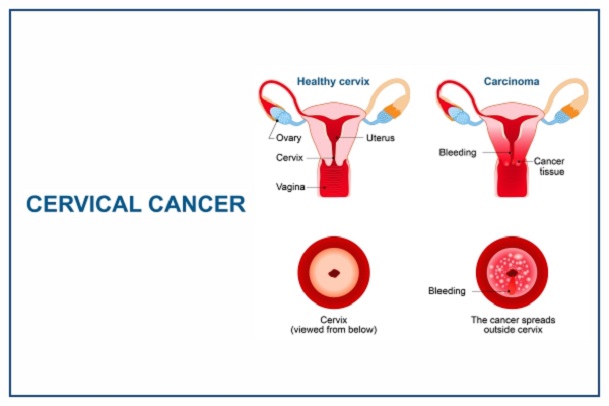
Cancer of the cervix (cervical cancer) is a type of cancer that occurs in the cells of the cervix i.e., the lower part of the uterus that connects to the vagina. When the cells in this part of the body begin to grow out of proportion and control, it leads to cancer of the cervix.
Who Has Cervical Cancer?
Cervical cancer affects only the female gender, being the only gender with a cervix. According to the World Health Organization (WHO), It is the fourth most frequent cancer in women with an estimated 604,127 cases in 2020. Of the estimated 342,000 deaths from cervical cancer in 2020, about 90% of these occur in low- and middle-income countries.
Women living with HIV are 6 times more likely to develop cervical cancer compared to women without HIV, and an estimated 5% of all cervical cancer cases are attributable to HIV.
What Causes Cervical Cancer?
Most cases of cervical cancer are usually caused by the sexually transmitted Human Papillomavirus (HPV). Most women get infected with HPV at some point but do not realize it. Though being affected by HPV does not mean a woman can get cervical cancer, but can if left untreated. In developed countries, HPV is not common among women. This is because early vaccination at aged 6 years and above is recommended. The vaccine against HPV helps create antibodies that reject and fight against the virus once contracted.
Other factors include:
Having a family History of Cervical Cancer: Once there is a family history of cervical cancer especially if the mother or sister had cervical cancer, the chances of developing the disease are higher than people with no family history of the disease.
Sexual History: Several factors related to a woman’s sexual history can increase the risk of cervical cancer. The risk is most likely affected by increasing the chances of exposure to HPV.
Having a Weakened Immune System: Human immunodeficiency virus (HIV), the virus that causes AIDS, weakens the immune system and puts people at higher risk for HPV infections. Another group of women at risk for cervical cancer are those who have not been vaccinated and taking drugs to suppress their immune response, such as those being treated for autoimmune disease (in which the immune system sees the body's tissues as foreign and attacks them, as it would a germ) or those who have had an organ transplant. Also, unvaccinated pregnant women who continue to engage in sexual activities are at risk of contracting HPV due to their weak immune systems.
Preventing Cancer of the Cervix
Cancer of the cervix is one of the preventable cancers in the world today, yet the lack of accurate information about its prevention has caused so many deaths, especially among women in Nigeria.
There are two ways of preventing cancer of the cervix i.e., primary and secondary forms of prevention.
Primary Form of Prevention
HPV Vaccination
The primary form of prevention is getting immunized against the human papillomavirus (HPV) infection. The preventive measure that can be taken against HPV is the HPV Vaccine. This vaccine should be routinely given to children (either male or female) who are below the age of 12 years (pre-teen) before their exposure to HPV.
This vaccine creates antibodies that protect them from contracting the virus when they grow up to have partners who are unvaccinated and have the HPV infection and become sexually active.
This vaccine does not protect individuals who are already infected with HPV because they cannot receive the vaccine after getting infected, but rather the vaccine has been shown to prevent infection with the types of HPV that cause most cervical cancers in women.
Getting the HPV vaccine while pregnant does not have any harmful effects on the pregnancy. People who are HPV-negative after getting screened, above the age of 21 years, and unvaccinated, can be given the HPV vaccine to protect them from the virus.
HPV vaccination does not replace cancer of the cervix screening. In countries where the HPV vaccine is introduced, screening programs population-based screening programs are needed to identify and treat cervical pre-cancer and cancer to reduce cancer of the cervix incidence and deaths.
HPV Vaccines: What You Need to Know
Human papillomavirus (HPV) vaccines are vaccines that prevent infection by the human papillomavirus. In a recommendation signed by The World Health Organization (WHO), HPV vaccines should be a part of routine vaccinations in all countries, along with other prevention measures. The vaccines require two or three doses depending on a person's age and immune status. Vaccinating children around the ages of 9 – 12 years is typically recommended. The vaccines protect for at least 5 to 10 years.
HPV vaccines are used to prevent HPV infection and therefore cervical cancer in women. There are currently two most widely used vaccines in the world i.e., Gardasil and Cervarix.
Who Should Get HPV Vaccination?
Regarding the age at which these vaccines could be administered, it was recommended that:
NOTE: When Gardasil was first introduced, it was recommended as prevention for cervical cancer for women that were 25 years old or younger. Evidence over the years has suggested that HPV vaccines are effective in preventing cervical cancer for women up to 45 years of age.
How Does The HPV Vaccines Work?
After an individual has been vaccinated, the vaccine creates antibodies that protect them from the HPV infection even if they become sexually active, and have partners who are HPV-positive. But once an individual (male or female) has become infected with HPV, the vaccine is no longer needed but rather secondary preventive methods are applied.
The vaccines do not prevent other sexually transmitted diseases, nor do they treat existing HPV infections or HPV-caused diseases.
How Effective Are HPV Vaccines?
HPV vaccines are highly effective in preventing infection with the types of HPV they target when given before initial exposure to the virus—which means before individuals begin to engage in sexual activity.
In the trials that led to the approval of Gardasil and Cervarix, these vaccines were found to provide nearly 100% protection against persistent cervical infections with HPV types 16 and 18 and the cervical cell changes that these persistent infections can cause. Gardasil 9 is as effective as Gardasil for the prevention of diseases caused by the four shared HPV types (6, 11, 16, and 18). The trials that led to the approval of Gardasil 9 found it to be nearly 100% effective in preventing cervical, vulvar, and vaginal disease caused by the five additional HPV types (31, 33, 45, 52, and 58) that it targets. In 2017, the World Health Organization stated that the HPV vaccines have equivalent efficacy. The Cervarix vaccine has been found to provide partial protection against a few additional HPV types not included in the vaccine that can cause cancer, a phenomenon called cross-protection.
To date, protection against the targeted HPV types has been found to last for at least 10 years with Gardasil, at least 9 years with Cervarix, and at least 6 years with Gardasil 9. Long-term studies of vaccine efficacy that are still in progress will help scientists better understand the total duration of protection.
How Safe Are These Vaccines?
The HPV vaccine is generally safe with no increased risk of serious adverse effects. HPV vaccines are approved for use in over 100 countries, with more than 100 million doses distributed worldwide. Although HPV vaccines are safe when given to people who are already infected with HPV, the vaccines do not treat the infection. They provide maximum benefit if a person receives them before he or she is sexually active.
Secondary Form of Prevention
The secondary form of prevention includes the use of screening methods for early detection and treatment of pre-cancerous lesions. Screening tests such as HPV and Pap tests are the most used for cancer of the cervix. This form of prevention is a cost-effective strategy to reduce the incidence and mortality of cervical cancer i.e., it might be quite expensive for low-income women.
Screening involves testing for HPV infection to detect pre-cancer and cancer, followed by treatment as appropriate. Testing is done among women who have no symptoms and may feel perfectly healthy. When screening detects an HPV infection or pre-cancerous lesions, these can easily be treated and cancer can be avoided. Screening can also detect cancer at an early stage where treatment has a high potential for cure.
Screening should start from 30 years of age in the general population of women, with regular screening with a validated HPV test every 5 to 10 years, and from 25 years of age for women living with HIV. Women living with HIV also need to be screened more frequently, every 3 to 5 years.
NOTE: When a pap test is positive and a cone biopsy of the cervix shows early changes in a grown woman who has had all her children, it is advisable to carry out a total hysterectomy to prevent the onset of full-blown cancer of the cervix.
Cervical Cancer in Nigeria/Africa vs Developed Countries
Cervical cancer is the most common genital cancer and one of the leading causes of death among the female population in Africa, especially in Nigeria. Although readily detectable in its early stage, cervical cancer remains the second most common cancer among women in Nigeria.
Among the female population in Nigeria, it was reported that 53.3 million women aged ≥15 years in Nigeria are at risk of developing cervical cancer with a current estimate indicating that every year 12,075 women are diagnosed with cervical cancer and 7968 die from the disease, giving a standardized prevalence rate of 33.0 per 100,000.
In Africa, cervical cancer is Swaziland, and Malawi has a very high cervical cancer rate compared to other African countries or the rest of the world (check Table 1 below). In contrast to this, in developed countries such as the United States of America (USA) and the United Kingdom (UK), the prevalence of cervical cancer among women is quite low due to the incidence rate between 7.3 and 9.4 per 100,000. This difference in the prevalence rate between African countries and most developed countries is due to the vaccination of children against HPV infection between the ages of 6 – 14 years in these developed countries before they are sexually active.
In developed countries such as the USA and the UK, HPV vaccination is free and routinely given to children before their teenage years (9 – 12 years). It is compulsory and has been included in their immunization programs for children.
According to NHS England, girls and boys aged 12 to 13 years (born after 1 September 2006) are offered the human papillomavirus (HPV) vaccine as part of the program. They are routinely offered the 1st HPV vaccination when they're in school Year 8. The 2nd dose is offered 6 to 24 months after the 1st dose.
It is important to have both doses of the vaccine to be properly protected. For those who are eligible and miss the HPV vaccine offered in Year 8 at school, it is available for free on the NHS up until your 25th birthday for:
In 2014, the South African government introduced free vaccinations against HPV to girls in public schools through the Integrated School Health Programme.
Health officials from the Department of Health visit government schools to carry out the HPV vaccination campaign. In 2023, the campaign aims to vaccinate all Grade 5 girls who are 9 years and older.
For a child to receive their vaccination, and be protected against cervical cancer and measles, parents or caregivers need to fill in and sign the consent forms that they will receive from their child’s school. No girl will be vaccinated without parental consent.
Therefore, vaccination of children with HPV vaccines before the onset of sexual activity is the most effective long-term intervention for reducing the risk of developing HPV and cancer of the cervix in women.
|
Table I – Age-Standardized Incidence Rate in African Countries |
||
|
Rank |
Country |
Age – Standardized Rate Per 100,000 |
|
1 |
Swaziland (Eswatini) |
84.5 |
|
2 |
Malawi |
67.9 |
|
3 |
Zambia |
65.5 |
|
4 |
Tanzania |
62.5 |
|
5 |
Zimbabwe |
61.7 |
|
6 |
Lesotho |
56.8 |
|
7 |
Uganda |
56.2 |
|
8 |
Comoros |
56.0 |
|
9 |
Mozambique |
50.2 |
|
10 |
Guinea |
50.1 |
|
11 |
Madagascar |
48.2 |
|
12 |
Burundi |
46.9 |
|
13 |
Burkina Faso |
45.1 |
|
14 |
Mali |
43.9 |
|
15 |
South Africa |
40.1 |
|
16 |
Senegal |
39.8 |
|
17 |
Liberia |
38.8 |
|
18 |
Angola |
37.2 |
|
19 |
Kenya |
35.6 |
|
20 |
Nigeria |
33.0 |
|
Table I – Age-Standardized Incidence Rate in Selected Developed Countries |
||
|
Rank |
Country |
Age – Standardized Rate Per 100,000 |
|
1 |
United Kingdom |
9.6 |
|
2 |
Germany |
8.9 |
|
3 |
Canada |
8.4 |
|
4 |
U.S.A. |
8.2 |
HPV Vaccination Situation in Nigeria
In the year 2016, the National Strategic Plan on Prevention and Control of Cervical Cancer in Nigeria highlighted the importance of vaccinating girls between the ages of 9 – 13 years against the Human Papillomavirus. They intended to leverage high-volume catchment areas toward delivering two doses of quadrivalent HPV vaccine to 4.5 million girls aged 9-13 years over 5 years at a financial cost of $18 million (USD). Similarly, the National Cancer Control Plan boldly set an objective of attaining 90% HPV vaccine coverage for girls aged 9-13 years in Nigeria by 2022. Although these ambitious goals were never achieved, they served as the foundation for future national cervical cancer prevention plans, especially HPV vaccine introduction.
On July 14, 2022, Faisal Shuaib, executive director of the National Primary Health Care Development Agency (NPHCDA), announced that HPV vaccines for Nigerian girls (9-14 years) will be introduced into Nigeria's expanded immunization program by the third quarter of 2023.
On the 29th of April 2023, The World Health Organization Country Representative in Nigeria, Dr. Walter Mulombo, the Human Papillomavirus vaccine would be introduced in the country by November 2023. If this situation is achieved, Nigeria would be joining some African countries like South Africa, Rwanda, Seychelles, Sierra-Leone, Kenya, Senegal, Malawi, Zimbabwe, Libya, Lesotho, Uganda, Botswana, and Mauritius who have introduced the HPV vaccine into their routine immunization schedules.